The World Health Organization (WHO) has updated its fact sheet on Maternal Mortality.
Background Information:
Maternal death is the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes.
Women die as a result of complications during and following pregnancy and childbirth. Most of these complications develop during pregnancy and most are preventable or treatable. Other complications may exist before pregnancy but are worsened during pregnancy, especially if not managed as part of the woman’s care. The major complications that account for nearly 75% of all maternal deaths are:
- severe bleeding (mostly bleeding after childbirth)
- infections (usually after childbirth)
- high blood pressure during pregnancy (pre-eclampsia and eclampsia)
- complications from delivery
- unsafe abortion.
The remainder are caused by or associated with infections such as malaria or related to chronic conditions like cardiac diseases or diabetes.
Most maternal deaths are preventable, as the health-care solutions to prevent or manage complications are well known. All women need access to high quality care in pregnancy, and during and after childbirth. Maternal health and newborn health are closely linked. It is particularly important that all births are attended by skilled health professionals, as timely management and treatment can make the difference between life and death for the mother as well as for the baby.
Severe bleeding after birth can kill a healthy woman within hours if she is unattended. Injecting oxytocics immediately after childbirth effectively reduces the risk of bleeding.
Infection after childbirth can be eliminated if good hygiene is practiced and if early signs of infection are recognized and treated in a timely manner.
Pre-eclampsia should be detected and appropriately managed before the onset of convulsions (eclampsia) and other life-threatening complications. Administering drugs such as magnesium sulfate for pre-eclampsia can lower a woman’s risk of developing eclampsia.
To avoid maternal deaths, it is also vital to prevent unwanted pregnancies. All women, including adolescents, need access to contraception, safe abortion services to the full extent of the law, and quality post-abortion care.
The main factors that prevent women from receiving or seeking care during pregnancy and childbirth are:
- poverty
- distance to facilities
- lack of information
- inadequate and poor quality services
- cultural beliefs and practices.
To improve maternal health, barriers that limit access to quality maternal health services must be identified and addressed at both health system and societal levels.
In the context of the Sustainable Development Goals (SDG), countries have united behind a new target to accelerate the decline of maternal mortality by 2030. SDG 3 includes an ambitious target: “reducing the global MMR to less than 70 per 100 000 births, with no country having a maternal mortality rate of more than twice the global average”.
Key Messages:
Every day in 2017, approximately 810 women died from preventable causes related to pregnancy and childbirth.
Between 2000 and 2017, the maternal mortality ratio (MMR, number of maternal deaths per 100,000 live births) dropped by about 38% worldwide.
94% of all maternal deaths occur in low and lower middle-income countries.
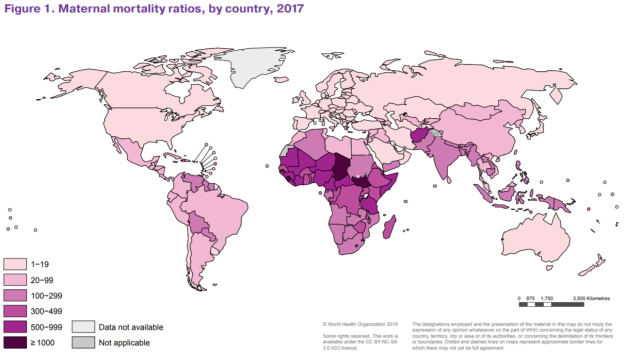
Sub-Saharan Africa and Southern Asia accounted for approximately 86% (254 000) of the estimated global maternal deaths in 2017. Sub-Saharan Africa alone accounted for roughly two-thirds (196 000) of maternal deaths, while Southern Asia accounted for nearly one-fifth (58 000).
At the same time, between 2000 and 2017, Southern Asia achieved the greatest overall reduction in MMR: a decline of nearly 60% (from an MMR of 384 down to 157). Despite its very high MMR in 2017, sub-Saharan Africa as a sub-region also achieved a substantial reduction in MMR of nearly 40% since 2000. Additionally, four other sub-regions roughly halved their MMRs during this period: Central Asia, Eastern Asia, Europe and Northern Africa. Overall, the maternal mortality ratio (MMR) in less-developed countries declined by just under 50%.
Nigeria and India had the highest estimated numbers of maternal deaths, accounting for approximately one third (35%) of estimated global maternal deaths in 2017, with approximately 67000 and 35000 maternal deaths (23% and 12% of global maternal deaths), respectively (India’s MMR was 145/ 100,000 live births in 2017). Three other countries also had 10 000 maternal deaths or more:
- The Democratic Republic of the Congo (16000),
- Ethiopia (14000) and
- The United Republic of Tanzania (11000).
Sixty-one countries were estimated to have had just 10 or fewer maternal deaths in 2017.
Women in less developed countries have, on average, many more pregnancies than women in developed countries, and their lifetime risk of death due to pregnancy is higher. A woman’s lifetime risk of maternal death is the probability that a 15 year old woman will eventually die from a maternal cause. In high income countries, this is 1 in 5400, versus 1 in 45 in low income countries.
Young adolescents (ages 10-14) face a higher risk of complications and death as a result of pregnancy than other women.
Skilled care before, during and after childbirth can save the lives of women and newborns.
Useful Links:
Link to the updated fact sheet:
https://www.who.int/news-room/fact-sheets/detail/maternal-mortality
Link to The Global Strategy for Women’s, Children’s and Adolescents’ Health (2016-2030):
https://www.who.int/life-course/partners/global-strategy/global-strategy-2016-2030/en/