Disclaimer: These maps are primarily intended for my students, but others may find them useful as well.
Note 1: As with all previous maps, feel free to download and share the maps for non-commercial use, but do mention the source (watermark notwithstanding).
Note 2: This programme emphasizes the continuum of care approach. As the strategy document provides a very good explanation of the same, I have reproduced the relevant passages verbatim below (quoted material) instead of trying to provide an alternative explanation.
Background Information:
Abbreviations used:
- IMR: Infant Mortality Rate
- MMR: Maternal Mortality Rate
- MCH: Maternal and Child Health
- HIV: Human Immunodeficiency Virus
- PHC: Primary Health Centre
- CHC: Community Health Centre
- FRU: First Referral Unit
- ANC: Antenatal Care
- STIs: Sexually Transmitted Infections
- RTIs: Reproductive Tract Infections
- IUCD: Intra-Uterine Contraceptive Device
- LSCS: Lower Segment Caesarean Section
Rationale, and the Continuum of Care concept:
“In order to bring greater impact through the RCH programme, it is important to recognise that reproductive, maternal and child health cannot be addressed in isolation as these are closely linked to the health status of the population in various stages of life cycle.
The health of an adolescent girl impacts pregnancy while the health of a pregnant woman impacts the health of the newborn and the child. As such, interventions may be required at various stages of life cycle,which should be mutually linked. The reasons for adopting such a strategy can be understood when the available data is taken into account and the close inter-linkages between different stages of life cycle are recognised.
Birth weight is an important risk factor for child survival as children with low birth weight (LBW) are more likely to have impaired growth, higher mortality and risk of chronic adult diseases. LBW is also a strong predictor for size in later life as most of these babies have intrauterine growth retardation, and they seldom catch-up with normal size during childhood. In India, 22% babies born each year have LBW, which has been linked to maternal under-nutrition and anaemia among other causes.
The mother’s condition before pregnancy is a key determinant of its outcome; half of adolescents (boys and girls) have below normal body mass index (BMI) and almost 56% of adolescent girls aged 15–19 years have anaemia. Therefore, the nutritional status of adolescent girls and young women is inextricably linked to the birth weight of their children and subsequently to child survival. There is evidence to show that adolescent mothers are vulnerable to problems related to pregnancy and childbearing. Of all mothers, adolescent mothers are more likely to have preterm births. According to national surveys, adolescents (15–19 years) contribute about 16% of total fertility in the country and 15–25 years age group contributes 45% of total maternal mortality.
With substantial unmet need of contraception – about 27% among married adolescents (15– 19 years) – and low condom use by adolescents in general, adolescent girls are at a high risk of contracting sexually transmitted infections, HIV and unintended and unplanned pregnancies. This in turn contributes to maternal morbidity and mortality due to unsafe abortions and infections.
High maternal and child mortality in adolescent mothers and a smaller but significant contribution of adolescents to total fertility brings the focus back on the need to address adolescents as an integral part of the strategy so as to improve maternal and child health.
Another compelling reason to invest in an integrated strategy across life stages is the well-known link between maternal and child survival,and the use of family planning methods. There is evidence to show that in developing countries, the risk of premature delivery and LBW doubles when conception occurs within six months of a previous birth. The use of contraceptive has the potential to improve perinatal outcomes and
child survival by widening the interval between successive pregnancies. Increased contraceptive use can also reduce the number of maternal deaths by reducing unintended pregnancies and thereby abating the number of times women face the hazards of pregnancy. Especially in areas with poor health infrastructure, family planning is a cost-effective and feasible way to reduce maternal and child deaths as it does not rely on complex technology. It is estimated that if the current unmet need for family planning could be fulfilled within the next five years, India can avert 35,000 maternal deaths and 12 lakh infant deaths while saving more than 4,450 crore of Indian currency. If safe abortion services are coupled with increase in family planning services, the savings made to the country could be to the tune of Rs 6,500 crore.
Just as different stages in the life cycle are interdependent so are the aspects of where and how healthcare is provided. Household or community education contributes to preventing health complications, quality care provided at the community level helps avoid the need for hospitalisation, and sound referral systems at primary care level support early identification of risks and better treatment for acute and complicated conditions. Essential interventions to improve the health of women and children therefore need to take place at all levels in the health system, that is, from the
home to the community level and through all the health facilities.
Thus, there are two dimensions to healthcare:
- stages of the life cycle and
- places where the care is provided.
These together constitute the ‘Continuum of Care.’ This Continuum of Care approach of defining and implementing evidence-based packages of services for different stages of the lifecycle, at various levels in the health system,has been adopted under the national health programme.”
Key Messages:
This article presents details of the Reproductive, Maternal, Newborn, Child and Adolescent Health (RMNCH+A) program that was launched in 2013.
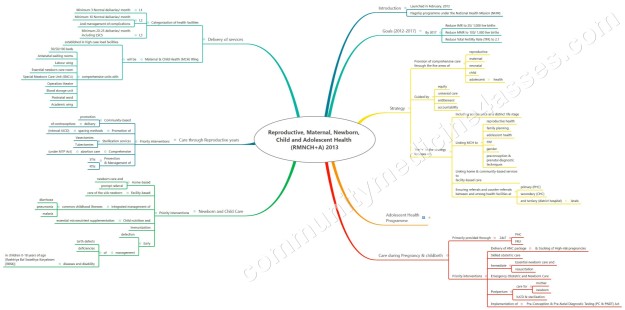
The ‘Plus’ in the strategic approach denotes the
- inclusion of adolescence as a distinct ‘life stage’ in the overall strategy;
- linking of maternal and child health to reproductive health and other components (like family planning, adolescent health, HIV, gender and Preconception and Prenatal Diagnostic Techniques (PC&PNDT); and
- linking of community and facility-based care as well as referrals between various levels of health care system to create a continuous care pathway, and to bring an additive /synergistic effect in terms of overall outcomes and impact.
The program seeks to further the continuum of care concept in Maternal and Child Health by linking all services from birth through a woman’s reproductive years.

It also introduces new initiatives like the use of Score Card to track the performance, National Iron + Initiative to address the issue of anemia across all age groups and the Comprehensive Screening and Early interventions for defects at birth , diseases and deficiencies among children and adolescents.
Useful Links:
Link to previous article on how to make sense of the mental maps:
https://communitymedicine4asses.com/2018/05/11/mental-maps-in-community-medicine-1-about-the-notes/
Link to RMNCH+A strategy document (English) [PDF]:
Click to access rmncha-strategy.pdf

